“Kia ora koutou katoa,” director-general of health Ashley Bloomfield says, opening the daily media briefing in Wellington on Monday, April 6. He confirms 39 new confirmed cases and 28 probables, taking the national total to 1106 cases.
“I also have a little bit more information about the new cluster in Christchurch I talked about yesterday,” he says. “This is associated with the Rosewood rest home.”
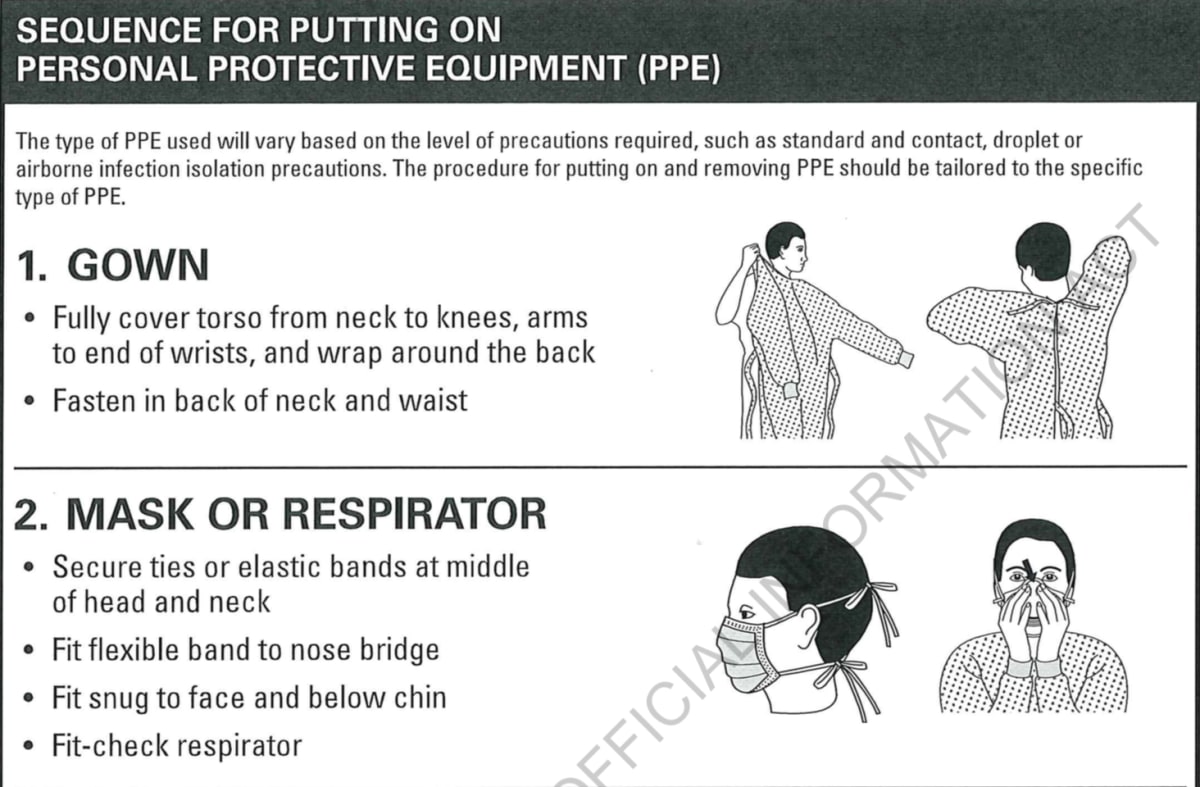
The rest home has 15 confirmed and probable cases, Bloomfield says – that’s four fewer than the figure mentioned the night before. The director-general touches on two major themes: PPE and staffing.
Moving the 20 Rosewood dementia unit residents to Burwood Hospital, which happened only hours earlier, is to “safely look after and isolate residents and also staff that facility”. (Rosewood comprises three wings – the dementia unit, rest home, and hospital.)
A Canterbury district health board (DHB) staffer has been appointed to supervise the care of the remaining residents, Bloomfield says, “to make sure that appropriate infection prevention control, including appropriate use of PPE, is happening there”.
(An early draft for Bloomfield’s update, shared between Canterbury DHB and Health Ministry communications staff, mentions both Christchurch aged care clusters – Rosewood and George Manning Lifecare and Village. The draft includes the line: “The DHB has kept the ministry informed about its work with both homes, and I am confident it is taking appropriate actions.” It doesn’t make the cut.)
How concerned is Bloomfield about the virus getting into Rosewood, considering it’s an aged care facility? He says the ministry is “very alert”, and is ensuring good supervision, and rigorous infection control and use of PPE. “Some of those remaining residents could be harbouring or incubating infections, so we want to make sure that they are well cared for.”
Back in Christchurch, there’s sensitivity and caution about what’s being said.
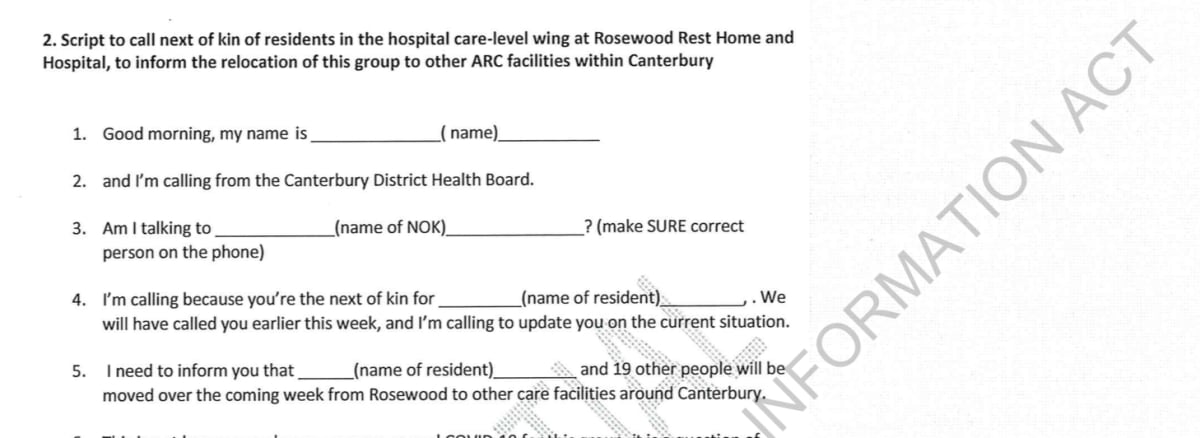
Eight minutes before the Wellington briefing starts, a draft script is circulated. It’ll will be read out, that afternoon, by DHB staff calling the families of Rosewood’s 44 remaining residents.
The words are as reassuring as possible. Initially, the script says there are no plans to move residents at this time. It’s suggested that should change to: “We have had all of our senior clinical teams assessing both the conditions and the status of the facility, and have also reviewed the residents, and we are not anticipating moving [patient’s name] at this time. Should anything change we will ring you as soon as possible.”
Despite the care and attention being paid to the “right messages”, some important missives are missed.
At about 3pm that Monday, a Fortè Health manager writes to chief medical officer Sue Nightingale, who’s one of the emergency coordination centre controllers, They ask for an update on Rosewood. The private hospital provided nurses to cover shifts at the two Covid-affected rest homes, and the manager’s aware DHB staff held a crisis meeting that morning.
“I am particularly interested to know whether my team members need to self-isolate or just social distance and whether testing would be available for them.”
(Another lapse is not telling emergency services immediately about Covid clusters, which prompts a grumpy email, later in the week, from Fire Emergency New Zealand to Civil Defence.)
With the dementia unit residents moved, the vacant Rosewood wing is shut. A “deep clean” is scheduled for later that week. Assurances are being given about attempts to secure “sustainable staffing” to care for the remaining residents. Strict hygiene procedures are in place, as is a new DHB-appointed manager, and there’s oversight from health experts.
But the rest home is still in disarray.
A DHB “work stream”, updated on Tuesday, April 7, says finding enough nurses to work there is a particular problem as there’s a “lack of willingness to work at Rosewood”. There just aren’t enough healthcare assistants, either.
A suggested way of reducing anxiety among CDHB staff who “see Rosewood as high risk” is to develop a communications plan.
With a national lockdown in place, and Easter weekend looming, the options to find staff are few and running out fast.
“There was dirty washing and incontinence nappies left on floors in some residents’ bathrooms, chairs in the dining room had food on them, floors needed a vacuum.” – External worker at Rosewood
On Tuesday morning, the alarm is sounded by contractor Ali’s Home Healthcare. After working Monday night at Rosewood, its most senior staffer, with many years’ experience in aged care, writes a long summary of problems, which is sent to the DHB emergency coordination centre’s “Covid staffing” address.
On arrival at the rest home, the Ali’s staffer says the night shift is told the only PPE they need is a mask, gloves, and hand sanitiser – “and you could change mask every 2hrs or so if you want”. Asked why full PPE isn’t provided, a male DHB staffer advises: “Infection control came in and said it wasn’t necessary”.
There is no handover from the day shift, so stand-in workers aren’t aware, until another person on night shift tells them, that day workers in the evacuated dementia unit also worked in the hospital wing. That mixing of units breaks DHB guidelines.
The DHB’s community and public health team clear some Rosewood workers to continue working. On that night shift, however, a doctor calls and tells one of them, a hospital wing caregiver, they shouldn’t be there and they’re not to go back.
Disregarding that advice, the caregiver stays for the full shift.
That’s lucky, the Ali’s staffer says, as there are not written instructions for each resident – their food, drink and care requirements. “We would have been completely blind.”
Across at the rest home wing, one carer is dedicated to a high-risk patient, leaving the other to do the “cares” and medication for 24 residents. A “DHB lady” hastily arranges help.
Back in the hospital wing, stand-in staff struggles include:
- There are only extra-extra-large incontinence nappies – which don’t fit all residents, so some leak, meaning beds have to be changed. That leads to extra, unnecessary contact;
- A registered nurse takes two hours to find medications;
- External staff don’t know how to transfer calls to the portable phone so residents can speak to families;
- Meals are left in a locked cooler outside, but staff aren’t initially told they’re there.
“The place wasn’t clean,” the senior staffer writes. “There was dirty washing and incontinence nappies left on floors in some residents’ bathrooms, chairs in the dining room had food on them, floors needed a vacuum.”
The Ali’s worker makes some common-sense suggestions, such as writing down each resident’s needs, and a task list for each shift, including where to find spare rubbish bags.
As the email is being digested, DHB communications staff prepare comments for Tuesday’s national press conference by “Ashley B & Jacinda” – Bloomfield and Prime Minister Jacinda Ardern.
Despite information on consecutive days that Rosewood staff have worked across different wings, the suggested line reads: “The residents are divided into two distinct areas/bubbles to ensure IPC guidelines and protocols are maintained.”
It doesn’t matter. No media at Tuesday’s briefing in Wellington ask about Rosewood.
The virus continues its spread. Of 11 positive cases in Canterbury on Tuesday, at least two are linked to Rosewood, including a family contact.
Eventually, the Christchurch rest home will become the country’s fourth most significant Covid cluster, with 55 cases.
It’s so much easier in retrospect.
A Health Ministry inquiry into significant Covid clusters at rest homes says when a staff member tests positive, a high proportion of the facility’s staff have to stand down. There are “limited prospects of backfilling these”. Their job’s made harder by “community misinformation, isolation from families and having their accommodation threatened by fearful landlords or housemates”.
Many frontline workers are haunted by news of “silent spreaders” – asymptomatic carriers who unknowingly pass on the virus.
On the morning of Wednesday, April 8, two days after Rosewood’s dementia wing residents are relocated, the potential risks of coronavirus spreading to another facility are raised.
The previous Saturday, a day after the first Rosewood case was confirmed, the same issue was raised by a manager from St George’s private hospital, which supplied nurses to cover shifts. Little fuss was made – they were sent two sets of guidelines.
But as the week wears on, trust in policy-following at Rosewood seems to wear thin – perhaps with good reason.
A DHB staffer emails a nurse manager on Wednesday morning. She points out a potential problem involving two family members, living together, working in healthcare. One works for Rosewood, the other an unidentified Christchurch charitable trust, which is thought to provide rehabilitation and lifestyle support services.
(The tip-off is prompted by discussion at that morning’s “welfare teleconference” – “apparently this is not the only instance of people from the same family unit working at different facilities”.)
After being approached, a trust representative undertakes to contact Rosewood’s temporary manager to establish “how trustworthy and appropriate the use of PPE was”. The manager “advised that no PPE was being worn in the dementia unit” – presumably before the first confirmed case.
Despite the Rosewood worker not having worked there for the last month they decide not to return to work this weekend, as the trust threatens to stand down their family member.
That’s a confusing tangle of messages.
Rosewood staff are being told that, with the dementia unit closed, the risk of transmission is so low they don’t have to wear full PPE. Yet a healthcare worker is at risk of being stood down because their family member, who “has not been at work for the last month”, might return to Rosewood.
Such angst isn’t evident in the draft DHB “communications pack” for fill-in Rosewood staff. (This appears to be the communications plan aimed at reducing staff’s anxiety.)
Fundamentally, workers must follow PPE guidelines, and adhere to hygiene and distancing measures. Do that, and show no symptoms, and they can return to their usual workplace after their temporary stint.
There’s a muddle, however, as the DHB wrestles with the tension between having to plug staffing gaps at Rosewood and uncertainty about being able to compel its own people to work there.
Guidance on “redeployment between facilities” says the Covid response might “require” staff to be temporarily deployed to other DHB facilities “or aged residential care (ARC) facilities”. It also says staff must “agree to be redeployed” after talking with their manager.
Legal advice settles the matter. Crown Law says the DHB can’t direct – force, basically – staff to work at Covid-affected rest homes.
With another avenue closed, the DHB starts planning for the worst-case scenario.
SOS to the military
The public messages being prepared are reasonably rosy.
A draft letter, dated Tuesday, to be sent in the name of Rosewood’s temporary manager, says staff “know what is expected of them”, have the necessary supplies and appropriate space to put on and remove protective equipment.
Yet a day later, as the staffing crisis worsens, the DHB sends a medical SOS to the military.
General manager of older persons Dan Coward, who’s another emergency controller, writes: “I have been requested by NHCC (the ministry’s National Health Coordination Centre) to place a request for support from NZDF medical teams.”
What’s required is supplementary staff – four to six registered nurses, 12 medics acting as heath care assistants, plus six staff for cleaning and other support. They’re to serve at Rosewood and another aged residential care (ARC) facility, presumably George Manning. Staff stand-downs have left 36 gaps in rosters.
“It is becoming increasingly difficult to staff, and support is required to sustain these two facilities over the next two weeks, enabling other plans to be developed and implemented to mitigate any further outcomes in other ARC facilities.”
The DHB has few options, Coward tells the military. It has ruled out moving the 86 residents from the two homes to hospital, “as it reduces our Covid response capacity and directs core staff away from core acute and non-deferrable care”.
All avenues have been exhausted with nursing agency firms. A request to one specialist database comes up blank; not one person completes vetting or other pre-employment checks.
The lack of a written reply suggests the Defence Force request fizzles out – which is a shame as the shambolic situation is about to get worse. More Rosewood residents are about to be moved.
Thursday, April 9, is a pivotal day at Rosewood.
The temporary manager leaves the facility, replaced by Alison Watkins, an experienced DHB service manager. Rosewood owners Malcolm and Lynda Tucker are sent a breach of contract notice. (The owners’ advocate, Mike Kyne, doesn’t respond to a request for comment.)
Three rest home wing residents are feverish – “but potentially non covid conditions”. They’re tested.
A DHB “workstream” on Rosewood paints a grim picture. “Unsustainable rosters as people do not turn up for shift. Issues of mixed messaging and previous lack of leadership.”
Crisis talks are held with nurses’ union NZNO.
Concerns include insufficient personal protective equipment (PPE), hand sanitiser, and inadequate gloves. A long-awaited stocktake of supplies at Rosewood is only completed that day.
(Despite the exposure risk being assessed as low, some Rosewood workers are wearing full PPE, clinical nurse specialist Suzy Rogers tells colleagues on Thursday. “We are happy for this to happen if it makes them feel confident to care for residents and maintains ability to provide ongoing staffing.”)
The union says there’s confusion about who’s in charge at Rosewood, and shift handovers are being done by inexperienced staff. Full overtime’s not being paid, it’s claimed. Also, some members are being worked too hard, the union complains. One staffer “has taken annual leave in order to get sufficient break between shifts”.
“These are also the issues we have been grappling with,” writes DHB nursing director care capacity demand Janette Dallas, adding it has “put things in place to resolve”.
However, it’s all come too late.
The decision’s made to move 20 hospital-level residents to other aged-care facilities. All of them are swabbed but results aren’t expected for 24-36 hours. That, no doubt, makes the frantic calls to other rest homes, to try and get them to take Rosewood residents, more difficult. (Some refuse to take any, and four facilities that initially say yes later renege.)
This might not have been the original plan. A draft press release from Thursday night, for what’s called “Rosewood Phase 2”, says 24 residents in the hospital-level care wing will be relocated, “along with one other person from Rosewood’s remaining dementia wing who now needs hospital-level care”.
In saying that, the rudder at Rosewood seems to shift, somewhat, away from chaos and towards order. With a new acting manager installed, and residents being moved, could it be the DHB is finally taking control?
Just after 5pm on Thursday an email delivers the news everyone has been dreading – the first death of a Rosewood resident at Burwood Hospital.
Scurrying again
Karalyn van Deursen, the DHB’s communications executive director, sends an email at 5.21pm on Thursday asking for the contact details of a family liaison person. They need to alert the family of the recently deceased woman the Health Ministry will announce the death of their loved one to the nation on Friday afternoon.
“The Director of Public health is likely to say that [redacted] had underlying health conditions, without going into details,” Van Deursen writes. The family is contacted before 8.30pm.
The ministry expresses an interest in the DHB also doing something to mark the death, like a live streamed media stand-up with medical officer of health Ramon Pink and chief medical officer Sue Nightingale. “I have managed to avoid that for now,” Van Deursen says.
Before the Rosewood residents are moved, a script is prepared for those phoning the families. “It is a question of staffing,” the callers say, adding the move is for the safety of residents.
Then there’s a bit of rest home roulette. Families are pointed to recent audits of rest homes on the Eldernet website. “We’ll give you some time to consider the options,” the script says. “When would suit to call you back?”
Is the relocation permanent? “That’s up to you,” says the script’s question and answer section. How long will this last? “We don’t know.”
It’s not clear when Rosewood might have sustainable hospital-level staffing again, the caller says pointedly. “We often find that once they are settled in their new environment and routine they are not keen to move again.”
Interestingly, the DHB’s frequently updated “Rosewood workstream” says Thursday’s decision is to “relocate the hospital level care patients permanently to other ARC facilities”.
An illustration of how quickly things are changing, or how hard it is to pull the numbers together, is the DHB’s tally of the Rosewood cluster’s numbers.
At 9.10am on Friday, it’s 20 cases, comprising eight staff and 12 patients. Less than half an hour before the 1pm briefing in Wellington, it’s suggested the staff cases are 16 (11 probable and five confirmed). Mid-afternoon, the finalised Canterbury DHB release puts it at 28 – and there are more staff affected than residents, 15 to 13, respectively.
Van Deursen writes: “Reconciling numbers betw cph [community and public health] and the moh is hurting my head.”

The DHB braces for a blowtorch of media interest.
Late on Friday morning, a chosen few are sent the Health Ministry’s draft press statement about the Rosewood-related death. It’s shared with the woman’s family, to ensure they’re comfortable with what’s being said.
Van Deursen says a short DHB statement will be provided “if asked”. The woman’s family has been told none of the information will identify her. But the comms supremo writes: “Media can be unscrupulous and go through social media etc looking for comments and clues.”
There is “significant media interest”, but it’s centred on the rest home itself. An email to the emergency managers at 2.40pm says: “URGENT security is needed at Rosewood due to media.”
Two external guards are sent, as are two DHB staffers to help field phone calls from families of Rosewood residents.
“Compared to the experience when the first death was announced on the West Coast we’ve had very little media interest,” Van Deursen writes just after 5pm. “And not one follow-up query to the relocating 20 additional residents – long may it remain that way.”
Mardi Postill, the team leader of older persons’ health, replies the residents’ families are happy to be contacted. “So positive about all the DHB was doing to support and helping to keep their loved [one] safe, really happy with the communication …. Thought I would pass that on as we often don’t hear the nice news!”
Late that afternoon, three new Rosewood-linked Covid-19 cases are confirmed. Then, just after 6pm, a doctor calls from Burwood Hospital’s ward GG – a second Rosewood resident, a man in his 70s, has died.
He aha te mea nui o te ao. He tāngata, he tāngata, he tāngata
The tragedy at Rosewood is about one thing, principally – people. The people who helped, those who became infected, the stressed staffers, and principled people who spoke up when presented with problems.
Most of all, it’s about the 12 residents who died and their families, many of whom couldn’t grieve in the normal way.
In Wellington’s Beehive theatrette on Friday, April 10, director of public health Caroline McElnay says the Rosewood resident who died at Burwood Hospital the previous day was aged in her 90s, and had underlying health conditions. She’d tested positive for Covid-19 earlier in the week.
“Because of the current level 4 [restrictions] no family members were able to visit the woman in hospital in recent days and were not able to be present when she passed away. However hospital staff were able to provide her with comfort and support and we thank them for that.”
* This narrative has been compiled from a 303-page Official Information Act response released to Newsroom, and publicly available sources.
Read part one of ‘Inside NZ’s deadliest cluster’ here



